Maximizing Heart Health Through Insightful BNP Test Results
Understanding How BNP Testing Plays a Crucial Role in Monitoring Heart Function

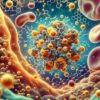
The information gained from BNP test results is incredibly valuable for the accurate detection and management of a wide range of cardiac conditions. This essential diagnostic test measures the amount of B-type Natriuretic Peptide (BNP), a hormone secreted by the heart in response to increased pressure, often signaling heart failure. Elevated BNP levels indicate the heart’s stress, providing insights into potential dysfunction that may need further investigation. A solid grasp of the importance of this test is crucial for both patients and healthcare providers, as it can significantly influence diagnostic and therapeutic strategies.
The BNP test is particularly relevant for individuals experiencing symptoms such as breathlessness, extreme fatigue, or swelling in the legs and arms. These clinical signs are often associated with heart-related disorders, making the BNP test an indispensable resource for healthcare professionals. It assists them in evaluating whether a patient’s heart is under significant stress and whether further diagnostic procedures or treatment plans are warranted. In addition, BNP testing is pivotal for assessing the effectiveness of heart failure treatments, offering crucial insights into a patient’s evolving health status over time.
Recognizing the significance of the BNP test is essential not only for those diagnosed with heart issues but also for individuals at risk for such conditions. Regular monitoring can facilitate timely medical interventions that greatly improve patient outcomes. The BNP test is a simple procedure that provides extensive information about a person’s cardiovascular health status.
Decoding BNP Levels: Key Insights for Assessing Heart Health
Achieving a thorough understanding of BNP levels is crucial for the accurate interpretation of the data obtained from BNP test results. Typically measured in picograms per milliliter (pg/mL), normal BNP levels are generally considered to be below 100 pg/mL. Levels exceeding this threshold can suggest heart failure or other cardiovascular issues. Nevertheless, it is vital to assess these results within a broader context, considering factors such as age, gender, and pre-existing health conditions.
For example, BNP levels in the range of 100 to 400 pg/mL may indicate a heightened risk for heart failure, but these numbers alone do not confirm a diagnosis. Levels surpassing 400 pg/mL typically point to more severe cardiac dysfunction. Furthermore, elevated BNP levels can also be affected by other medical issues, including kidney failure, respiratory conditions, or severe infections like sepsis. Therefore, it is essential for healthcare professionals to take the entire clinical picture into account when interpreting BNP levels.
Conversely, low BNP levels can also provide significant insights into cardiac health. While low levels generally indicate that heart failure is unlikely, they may sometimes be misleading if not evaluated in the context of the patient’s comprehensive health status. For instance, a patient could exhibit low BNP levels yet still display symptoms of heart failure due to other underlying health issues. Thus, a complete understanding of how to interpret BNP levels is critical for making informed healthcare decisions.
The Necessity of Continuous BNP Level Monitoring for Optimal Heart Health
Ongoing monitoring of BNP levels is vital for effectively managing cardiovascular health. Regular testing allows healthcare providers to track changes over time, offering essential data necessary for evaluating the progression of cardiac conditions or the effectiveness of treatment strategies. For patients with existing heart issues, routine BNP testing can alert physicians to any deterioration in health, enabling timely interventions that could be life-saving.
Beyond tracking existing conditions, regular BNP testing can also benefit individuals at elevated risk for heart failure. Those with risk factors such as hypertension, diabetes, or a family history of heart disease can particularly gain from ongoing BNP evaluations. These tests act as an early warning system, identifying potential health issues before they develop into more severe conditions.
Moreover, the importance of patient engagement in this process cannot be overstated. Educating patients about their BNP test results and the implications for their heart health encourages a proactive approach to care. When patients understand the significance of regular monitoring, they are more likely to adhere to testing schedules and follow medical recommendations. This collaborative relationship between patients and healthcare providers is fundamental to improving heart health outcomes.
Understanding Your BNP Test Results: Essential Insights for Better Health

Recognizing Normal BNP Levels: Indicators of a Healthy Heart
Normal BNP levels serve as reassuring indicators of effective heart function. Values below 100 pg/mL typically suggest that the heart is operating optimally and there is a low likelihood of heart failure. Such results indicate that the heart is effectively managing blood flow and pressure without undue stress, which is a hallmark of a healthy cardiovascular system.
It is essential for both patients and healthcare providers to understand the implications of being within the normal range. This comprehension extends beyond mere numerical values; it reflects the heart’s operational efficiency. For example, a patient whose BNP level is within the normal range but who is experiencing symptoms may require additional evaluations to rule out other health issues. This underscores the importance of integrating BNP results with clinical assessments and other diagnostic instruments to achieve a comprehensive view of heart health.
Moreover, achieving normal BNP levels can serve as an encouraging benchmark for individuals recovering from heart-related issues. A patient who had previously elevated BNP levels may find motivation in subsequent test results that return to normal. This improvement can signify effective treatment and a recovery trajectory for the patient’s heart health. Consistently achieving normal BNP results can also inspire patients to maintain healthy lifestyle choices, reinforcing the positive effects of their efforts on overall cardiovascular wellness.
Recognizing Elevated BNP Levels: Understanding Causes and Associated Health Risks
Elevated BNP levels often signify potential cardiac issues, particularly heart failure. When BNP levels exceed 100 pg/mL, it denotes increased pressure on the heart, frequently due to underlying conditions such as chronic obstructive pulmonary disease (COPD), kidney dysfunction, or acute coronary syndrome. The rise in BNP levels occurs as the heart exerts more effort to meet the body’s demands, indicating a decline in heart function.
Understanding the factors contributing to elevated BNP levels is crucial for effective management. For example, in patients with chronic heart failure, BNP levels can fluctuate based on the severity of their condition and how well their treatment plan is functioning. Significant increases may prompt healthcare providers to adjust medications, recommend lifestyle modifications, or consider additional diagnostic evaluations. This adaptability in treatment is vital for effectively managing chronic conditions.
In addition, elevated BNP levels can signify problems beyond the heart. For example, they may reflect renal complications, where the kidneys’ inability to filter waste efficiently can lead to increased BNP levels. Therefore, healthcare providers must evaluate the broader clinical context when interpreting elevated BNP results, ensuring that all potential contributing factors are taken into account.
Interpreting Low BNP Levels: Insights and Possible Concerns

While elevated BNP levels often receive considerable attention, understanding the implications of low BNP levels within the data derived from BNP test results is equally important. Levels below 100 pg/mL generally provide reassurance, suggesting that heart failure is unlikely. However, low BNP levels can occasionally be misleading, particularly in patients who present symptoms consistent with heart failure.
In some situations, a patient may exhibit classic heart failure symptoms despite having low BNP levels, indicating that the heart is functioning adequately. This scenario highlights the importance of a comprehensive diagnostic approach rather than relying solely on BNP results. Factors such as age, gender, and existing medical conditions can influence BNP levels, complicating their interpretation.
Low BNP levels may also be found in individuals who are very physically active or those who have recently engaged in intense exercise. In these instances, the body’s effective regulation of blood flow can result in decreased BNP production. Recognizing these nuances is crucial for healthcare providers to deliver accurate diagnoses and appropriate treatment plans.
Moreover, low BNP levels can empower patients to take control of their cardiac health. For those who have undertaken significant lifestyle changes—such as improving their diet, increasing physical activity, or adhering to prescribed medications—achieving low BNP levels can reinforce their commitment to maintaining cardiovascular health. In this context, low BNP levels can symbolize the success of proactive health management strategies.
Utilizing BNP Test Results for Empowered Health Choices
Recognizing When to Seek Medical Attention Based on BNP Insights
Understanding the appropriate time to consult a healthcare professional based on insights from BNP test results is critical for effective heart health management. Elevated BNP levels clearly signal that a healthcare provider should conduct a more thorough evaluation. If a patient’s results show BNP levels significantly exceeding the normal range, it is imperative to schedule a follow-up appointment promptly.
Patients should also be aware of symptoms that may accompany abnormal BNP levels. Signs such as persistent shortness of breath, swelling in the limbs, or rapid weight gain can indicate declining heart function and warrant immediate medical attention. Recognizing the relationship between BNP levels and these physical symptoms empowers patients to advocate for their health and seek timely interventions.
Moreover, even when BNP levels fall within normal limits, those at risk for cardiovascular diseases should maintain open lines of communication with their healthcare providers. Regular check-ups and BNP testing can aid in monitoring heart health and identifying changes early. Patients should feel encouraged to express their concerns and symptoms openly to ensure that potential issues are addressed before they develop into more serious health problems.
Ultimately, discerning the right moments to seek medical advice based on BNP results requires interpreting numerical data alongside personal health symptoms. This proactive approach is essential for sustaining optimal heart health and effectively managing any underlying issues.
Implementing Lifestyle Changes Based on BNP Test Findings
Embracing lifestyle modifications can significantly enhance heart health and are often recommended based on insights from BNP test results. For patients with elevated BNP levels, adopting heart-healthy lifestyle changes can assist in managing their condition and improving overall cardiac function. These changes typically include dietary adjustments, increased physical activity, and effective stress management techniques.
A heart-healthy diet emphasizes whole foods, such as fruits, vegetables, whole grains, and lean proteins, while minimizing processed foods, sodium, and saturated fats. Reducing sodium intake is especially crucial for individuals with elevated BNP levels, as it aids in controlling fluid retention and easing pressure on the heart. Collaborating with a registered dietitian can provide personalized dietary recommendations tailored to individual health needs.
Incorporating regular physical activity into daily routines is another critical aspect of heart health. Exercise strengthens the heart muscle, enhances circulation, and improves cardiovascular fitness. For patients with elevated BNP levels, a structured exercise program—often supervised by healthcare professionals—can lead to noticeable improvements in heart function. Simple activities like walking or swimming can yield substantial benefits.
Furthermore, managing stress is vital for maintaining heart health. Chronic stress can negatively affect cardiovascular function, contributing to elevated BNP levels. Techniques such as mindfulness, yoga, or regular relaxation exercises can help reduce stress and promote overall well-being. By prioritizing these lifestyle changes, patients can take proactive measures to improve their heart health and potentially lower their BNP levels over time.
Understanding How Medications Affect BNP Levels
Grasping the connection between medications and insights from BNP test results is essential for patients managing heart conditions. Certain medications can significantly influence BNP levels, either through direct improvement of heart function or by addressing underlying conditions that contribute to elevated BNP levels. For instance, diuretics, which are commonly prescribed for heart failure, can lower BNP levels by alleviating fluid overload in the body.
Patients should maintain transparent communication with their healthcare providers regarding their medication regimens, as some drugs may mask or alter BNP levels. For example, medications like ACE inhibitors or beta-blockers can enhance heart function, potentially leading to lower BNP levels over time. Understanding these relationships allows healthcare providers to interpret BNP results accurately and make informed treatment decisions.
It is also vital for patients to recognize that while medications can be beneficial, they should not be viewed as standalone solutions. An effective approach to heart health typically includes lifestyle modifications alongside pharmacological interventions. Patients should closely collaborate with their healthcare team to develop a personalized strategy that considers their unique health status, medication regimen, and lifestyle choices.
Ultimately, the interplay between medication and BNP levels underscores the importance of ongoing monitoring and communication with healthcare providers. By understanding how medications influence BNP levels, patients can engage more actively in their care and contribute to informed decision-making regarding their heart health.
Key Factors Affecting BNP Test Results: Understanding Variability
The Impact of Age and Gender on BNP Testing
Age and gender are significant factors in interpreting insights from BNP test results. BNP levels vary with age, as older adults typically exhibit higher baseline levels compared to younger individuals. This age-related increase in BNP can complicate the interpretation of results, particularly in older patients displaying symptoms suggestive of heart failure. As a result, healthcare providers must take age into account when evaluating BNP levels.
Gender also plays a role in BNP levels, with women usually having higher BNP levels than men, even in the absence of heart disease. This gender variation necessitates the establishment of gender-specific reference ranges for interpreting BNP test results. Healthcare providers must be cognizant of these differences to avoid misdiagnosis and ensure that all patients receive evaluations tailored to their unique physiological characteristics.
Understanding these demographic factors enhances the early identification of cardiovascular issues. For example, a woman in her sixties with slightly elevated BNP levels may warrant a different clinical approach than a younger man with similar levels. This personalized interpretation can enhance diagnostic accuracy and promote timely interventions.
As the population ages, the relevance of these considerations will only increase. With heart disease remaining a leading cause of morbidity and mortality among older adults, understanding how age and gender affect BNP levels is essential for improving patient outcomes and ensuring appropriate care is delivered.
The Role of Comorbidities in Influencing BNP Levels
A variety of health conditions can significantly impact insights from BNP test results, complicating the interpretation of BNP levels. Conditions such as kidney disease, pulmonary hypertension, and obesity can lead to elevated BNP levels, even without the presence of heart failure. For example, in patients with renal impairment, the kidneys’ inability to effectively excrete BNP can result in artificially high levels, potentially misleading healthcare providers regarding the patient’s cardiovascular health.
Obesity is another key factor influencing BNP levels. Adipose tissue produces inflammatory markers that can lead to elevated BNP levels independent of heart function. As a result, patients with obesity may show increased BNP levels, necessitating a comprehensive evaluation of their overall health status and other risk factors. This complexity emphasizes the importance of a holistic approach to interpreting BNP results, ensuring that all potential influences are taken into account.
Chronic lung diseases, such as chronic obstructive pulmonary disease (COPD), can also contribute to elevated BNP levels. The increased work of breathing and strain on the cardiovascular system associated with these conditions can lead to elevated BNP levels, mimicking symptoms of heart failure. Thus, healthcare providers must assess BNP results alongside other diagnostic tools and clinical evaluations.
Recognizing the impact of comorbidities on BNP levels is vital for accurate diagnosis and effective management. By considering the broader health context, healthcare providers can formulate comprehensive treatment plans that address both heart health and other interconnected health issues.
Best Practices for Timing and Frequency of BNP Testing
The timing and frequency of BNP testing are crucial for obtaining accurate and actionable insights into BNP test results. Regular monitoring of BNP levels can provide valuable insights regarding changes in cardiac function for patients with known heart conditions or those at elevated risk. The frequency of testing may vary based on the individual’s health status, treatment plan, and the severity of their condition.
Generally, patients with chronic heart failure may benefit from more frequent BNP testing, particularly during periods of treatment adjustments or symptom exacerbation. Routine testing enables healthcare professionals to track changes in BNP levels over time, ensuring timely interventions if levels begin to rise. Conversely, testing may be performed less often for patients with stable heart health and low BNP levels, provided there are no new symptoms or changes in health status.
Timing is also critical when interpreting BNP levels. Factors such as recent physical activity, stress, or acute illness can influence BNP levels and may result in temporary fluctuations. Consequently, healthcare providers often recommend testing at specific intervals to ensure consistency in results. For instance, testing may be conducted while fasting or following a period of rest to minimize external influences.
In summary, understanding the timing and frequency of BNP testing is essential for accurately monitoring heart health. By adhering to best practices for testing, patients and healthcare providers can ensure that BNP results provide meaningful insights into cardiovascular function and guide effective management strategies.
Real-Life Applications and Case Studies of BNP Test Insights
Case Study: Early Detection of Heart Failure Through BNP Testing
A compelling example of the value of BNP test result insights in clinical practice can be illustrated through the case of a 65-year-old female patient who presented with unexplained shortness of breath and fatigue. Initial evaluations revealed no apparent respiratory complications, prompting further investigation through BNP testing. The results indicated a BNP level of 520 pg/mL, significantly above the normal range.
This elevated BNP level prompted an immediate response from her healthcare team, leading to a thorough assessment of her cardiovascular function. Follow-up imaging studies revealed early signs of heart failure. Thanks to timely intervention—including medication adjustments and lifestyle recommendations—the patient was able to effectively manage her condition. Subsequent BNP testing over the following months demonstrated a gradual decline in her BNP levels, indicating improved heart function and a positive response to treatment.
This case exemplifies the crucial role of BNP testing in the early identification of heart failure. The ability to recognize heart failure in its initial stages, coupled with appropriate treatment strategies, can significantly enhance patient outcomes and quality of life. By leveraging BNP test result insights, healthcare providers can make informed decisions that directly impact patient health.
Managing Chronic Heart Conditions: The Indispensable Role of BNP Testing
For patients managing chronic heart conditions, BNP testing is a fundamental aspect of ongoing care and treatment. Consider the case of a 72-year-old male patient with a history of congestive heart failure. His treatment plan included regular BNP monitoring alongside medication management. Over time, fluctuations in his BNP levels were correlated with his symptoms and overall health status.
When BNP levels rose significantly, indicating worsening heart failure, his healthcare team promptly adjusted his treatment regimen. This included modifications to his medications and dietary recommendations. This proactive approach allowed the healthcare team to address concerns before they escalated, ultimately leading to improved patient outcomes.
Incorporating BNP test results into the patient’s ongoing management plan proved essential in this scenario. Regular BNP testing provided the healthcare team with actionable data that informed treatment decisions, ensuring the patient received timely and appropriate care. This case highlights the importance of continuous monitoring in managing chronic heart conditions and emphasizes the need for collaboration between patients and providers to optimize health outcomes.
The Critical Role of BNP Testing in Emergency Scenarios
The essential role of BNP testing in emergency departments cannot be overstated. Consider the case of a 58-year-old male who arrived at the emergency department with acute chest pain and shortness of breath. Initial assessments were inconclusive, and the medical team needed to quickly rule out potential cardiac complications. A BNP test revealed a level of 850 pg/mL, indicating significant heart strain.
This elevated BNP level prompted immediate action, including further cardiac evaluations and treatment for potential heart failure. The swift identification of elevated BNP levels enabled the medical team to implement life-saving interventions and stabilize the patient’s condition. This case underscores the urgent need for BNP testing in acute care settings, where prompt decision-making is critical.
By utilizing BNP test result insights, emergency healthcare providers can make informed decisions that directly impact patient care. The ability to quickly assess heart function through BNP testing enhances the overall efficiency of emergency medicine, ensuring that patients receive timely and appropriate interventions in critical situations.
The Future of BNP Testing: Innovations and Emerging Trends
Advancements in BNP Testing Technologies
As cardiovascular medicine continues to evolve, so does the technology surrounding BNP test result insights. Recent advancements in testing technology have enhanced the accuracy and speed of BNP testing, making it more accessible for healthcare providers and patients. New point-of-care testing devices facilitate rapid BNP measurements, allowing healthcare professionals to obtain results within minutes rather than hours.
These technological advancements are particularly beneficial in emergency scenarios, where timely decision-making is crucial. The ability to rapidly evaluate BNP levels can significantly influence patient management, enabling immediate therapeutic interventions when necessary. Additionally, laboratory testing techniques have improved the sensitivity and specificity of BNP assays, reducing the likelihood of false positives or negatives.
Furthermore, the integration of BNP testing with digital health technologies is an emerging trend. Wearable devices that monitor heart health and transmit data in real-time are becoming increasingly popular. These innovations can help bridge the gap between traditional testing methods and continuous monitoring, allowing for more dynamic management of heart health.
As technology progresses, the future of BNP testing holds immense promise for enhancing patient outcomes and improving healthcare delivery. By embracing these innovations, healthcare providers can leverage BNP test result insights to make informed decisions and optimize patient care.
Integrating BNP Testing with Holistic Diagnostic Strategies
Combining BNP testing with other diagnostic tools represents a pivotal trend in cardiovascular care. Healthcare providers are increasingly acknowledging that BNP levels should be assessed alongside other evaluations, including echocardiograms, electrocardiograms (ECGs), and clinical assessments.
Integrating BNP testing with imaging studies provides a more comprehensive view of a patient’s cardiovascular health. For instance, while BNP levels can indicate heart stress, an echocardiogram can yield detailed insights into heart structure and function. This multifaceted approach enhances diagnostic accuracy and allows healthcare providers to devise tailored treatment plans that address the complexities of each individual’s condition.
Moreover, combining BNP testing with additional biomarkers can refine risk assessment and management strategies. Ongoing research aims to identify supplementary biomarkers that may complement BNP testing, providing a more holistic perspective on cardiovascular health. This integration can lead to better-informed decisions regarding treatment options, lifestyle modifications, and monitoring strategies.
As cardiovascular medicine progresses, the collaborative use of BNP testing alongside other diagnostic tools will be essential for optimizing patient care. By leveraging BNP test result insights with comprehensive assessments, healthcare providers can enhance outcomes and improve the overall quality of care.
The Role of BNP Testing in Preventive Healthcare Initiatives
The increasing relevance of BNP testing in preventive medicine is being recognized within the healthcare community. As individuals become more invested in their heart health, BNP testing can serve as a valuable resource for early detection and risk stratification. For individuals with risk factors for heart disease, regular BNP testing can reveal potential issues before they escalate into serious health concerns.
Preventive medicine focuses on identifying and mitigating risks to enhance long-term health outcomes. BNP testing aligns seamlessly with this philosophy by providing actionable insights into heart health that can inform lifestyle changes and treatment strategies. For example, individuals with elevated BNP levels may benefit from targeted interventions, such as dietary modifications, increased physical activity, and medication management, to reduce their risk of developing heart failure.
Furthermore, incorporating BNP testing into routine health assessments can empower patients to take charge of their cardiovascular health. By understanding their BNP levels and the implications for heart health, individuals can proactively discuss prevention strategies with their healthcare providers. This collaborative approach fosters a culture of health awareness, motivating individuals to prioritize their cardiovascular well-being.
In conclusion, the role of BNP testing in preventive medicine is expanding as healthcare providers recognize its potential for early detection and risk management. By utilizing BNP test result insights as part of a comprehensive preventive health strategy, patients can take proactive steps to optimize their cardiovascular health and reduce the risk of heart-related complications.
Common Questions and Concerns About BNP Testing Addressed
Assessing the Reliability of BNP Tests
BNP tests are generally regarded as reliable; however, various factors can impact their accuracy. Fluctuations in results may arise from individual health issues, medications, and testing methodologies. Healthcare providers must consider these elements when interpreting BNP levels.
Understanding the Variability in BNP Levels
BNP levels can fluctuate due to numerous factors, including physical activity, stress, or acute illness. Continuous monitoring of BNP levels over time is essential for recognizing trends rather than relying on a single measurement.
BNP Testing Considerations for Different Age Groups
BNP testing should be adjusted according to specific age demographics, as baseline levels can significantly differ among children, adults, and the elderly. Healthcare providers must factor in age-related considerations when interpreting results.
Next Steps Following Elevated BNP Levels
If your BNP levels are elevated, it is critical to consult with your healthcare provider. They will assess your overall health, symptoms, and underlying conditions to develop an appropriate management plan.
Potential Risks Associated with BNP Testing
BNP testing is a straightforward blood test with minimal risks. However, as with any blood draw, there may be slight discomfort or bruising at the needle site, although serious complications are rare.
Determining the Frequency of BNP Testing
The frequency of BNP testing varies depending on individual health conditions and risk factors. Those with heart failure or significant risk factors may require more frequent testing, while others may undergo testing annually or as symptoms arise.
Lifestyle Changes That Can Affect BNP Levels
Modifications to lifestyle, such as improved nutrition, increased physical activity, and effective stress management, can positively influence BNP levels. These adjustments may lead to enhanced heart health and lower BNP readings.
Complementary Tests That Enhance BNP Testing
BNP testing is often utilized in conjunction with other diagnostic tools, including echocardiograms and ECGs, to conduct a thorough assessment of heart health. This integrated approach improves diagnostic accuracy.
Insurance Coverage for BNP Testing
Most insurance plans cover BNP testing, particularly when deemed medically necessary. Patients should confirm coverage details with their insurance provider to understand potential out-of-pocket expenses.
Preparation Guidelines for BNP Testing
No specific preparation is necessary for a BNP test. However, it is advisable to inform your healthcare provider about any medications and recent health changes that may affect test results.
Connect with us on Facebook for exclusive updates!
This Article Was First Found On https://bloodtest.co.uk
The Article: BNP Test Insights for Enhanced Health Understanding appeared first on: https://ezbloodtest.com
The Article BNP Test Insights to Improve Your Health Awareness Was Found On https://limitsofstrategy.com
The Article BNP Test Insights for Enhanced Health Awareness First Appeared ON
: https://ad4sc.com







Comments are closed